What you’ll learn:
- Menopause-related hormone changes can significantly impact your sleep, leading to issues like insomnia, night sweats, and sleep apnea.
- Hormone replacement therapy (HRT) and over-the-counter remedies can provide relief but always weigh the benefits and risks with a healthcare provider.
- Lifestyle changes, such as maintaining a consistent sleep schedule and creating a relaxing sleep environment, can significantly improve sleep quality during menopause.
Menopause brings plenty of changes, and unfortunately, sleep issues are often part of the package. When hormones start to fluctuate, they can throw your sleep patterns off, leading to night sweats, mood swings, and stress that can make your nights less than restful. A good night’s sleep can feel like a distant memory during menopause, but you’re not alone. Many women going through menopause find themselves counting sheep more often than they’d like.
Getting enough quality shut-eye isn’t just about avoiding under-eye circles—it’s a big deal for your overall health. We’ve gathered some tips to help you catch more Z’s and guidance on where to turn if you need to explore hormone replacement therapy and other therapies.
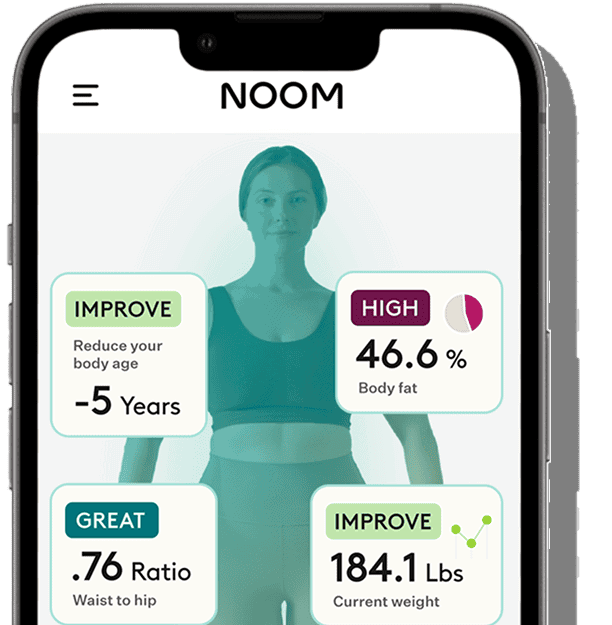
At Noom, we know that feeling your best starts with the basics, like a good night’s rest. Here are the ways to wake up feeling more like yourself.
Understanding how hormone changes affect sleep during menopause
As you approach menopause, your hormones, particularly estrogen and progesterone, can begin to fluctuate as your ovaries begin to run out of eggs. You may start feeling the effects in your 40s during perimenopause, the time period that leads up to menopause. Before you officially reach menopause, 12 months after your last menstrual period, is when hormonal fluctuations can be quite dramatic.
Erratic hormone levels can disrupt sleep patterns, causing you to wake up at night and have trouble falling asleep. Why do these hormones typically associated with fertility affect your sleep? Let’s break it down:
Estrogen: Your body’s sleep regulator
Estrogen is one of the big players when it comes to sleep, and its decline during menopause can really shake things up. Here’s what it does:
- Temperature regulation: As estrogen levels drop, many women experience hot flashes and night sweats. These sudden temperature changes can wake you up and make it hard to fall back asleep, disrupting your rest. Research shows that estrogen affects temperature regulation in different parts of the body, sometimes working together or in opposing ways, which can contribute to these temperature shifts during menopause.
- Sleep length: Estrogen also influences neurotransmitters like serotonin and norepinephrine, which are responsible for regulating your sleep-wake cycles, according to a review study. When estrogen dips, you may find yourself having trouble falling asleep or staying asleep. Estrogen drop may lead to longer sleep onset (meaning it takes longer actually to fall asleep) and more frequent wake-ups in the night.
- Sleep quality: Estrogen supports deeper, more restorative sleep, according to this study. When estrogen levels decline, you might notice that you’re waking up feeling unrefreshed, even after a full night’s sleep.
Progesterone: The natural sleep aid
Often called the “sleep hormone,” progesterone has a natural calming effect on the body, and it plays a big role in helping you drift off into restful sleep. Here’s how it impacts your rest:
- Sedative effects: Progesterone acts on the brain’s GABA receptors, which are involved in reducing anxiety and promoting relaxation. As progesterone decreases during menopause, it becomes harder for your body to relax and fall asleep.
- Sleep stages: Progesterone also helps you maintain those deeper sleep stages. When progesterone levels fall, sleep can become more fragmented, making it difficult to stay asleep for long stretches of time.
- Respiratory function: Another crucial role progesterone plays is in regulating breathing during sleep. Researchers found that progesterone’s decline can contribute to issues like obstructive sleep apnea (OSA), which interrupts your sleep and leaves you feeling even more tired the next day.
Follicle-stimulating hormone (FSH): The menopause marker
FSH might not be as well-known, but it’s another hormone that plays a key role in your sleep patterns during menopause. Here’s why:
- Increased FSH = more wakefulness: As menopause approaches, FSH levels rise because the ovaries produce fewer hormones. This increase in FSH is linked to more wakefulness during the night. A study found that higher FSH levels were connected to more frequent awakenings and lighter sleep in perimenopausal people, even without sleep complaints. The same study showed that higher FSH levels in premenopausal people were also associated with lighter sleep.
- FSH as a menopause indicator: FSH levels are also a marker of the menopausal transition. The fluctuations in FSH levels signal the changes happening in your body, and they often coincide with other menopausal symptoms like hot flashes. So, the rise in FSH can directly contribute to sleep struggles during this time.
So, what does this all mean for you? Essentially, as your hormone levels shift, your body’s ability to regulate sleep, maintain deep rest, and stay asleep could get disrupted. But knowing what’s happening behind the scenes gives you the power to take action, adjust your routine, and manage your sleep struggles with the right strategies.
Common sleep disturbances during menopause
The combination of hormonal changes and other factors makes it harder to sleep through the night, and many women end up facing a variety of sleep struggles. Here’s a look at the most common sleep disturbances that crop up during this time:
- Hot flashes and night sweats: Hot flashes are sudden bursts of heat that can leave you tossing and turning, especially at night when they’re called night sweats. About 75-85% of women experience hot flashes or night sweats during menopause. These temperature spikes, caused by hormonal shifts, can cause sudden awakenings and make it tough to get back to sleep.
- Insomnia: Struggling to fall or stay asleep or waking up way too early? That’s insomnia, and it becomes more common during menopause. Both hormonal changes and psychological factors like anxiety and depression play a big role in this. Research suggests about 26% of perimenopausal people struggle with insomnia, with the most common symptom being difficulty staying asleep throughout the night.
- Restless legs syndrome (RLS): RLS is a condition that makes a person need to move their legs. That irresistible urge to move might bring temporary relief, but it can also disrupt sleep. A study found that 53% of women dealing with sleep issues had conditions like RLS or sleep apnea. What’s the connection to menopause? Hormonal fluctuations during menopause, especially changes in estrogen levels, may influence dopamine and glutamate transmission in the brain, both linked to RLS. Regional brain iron deficiency is more common in women, and comorbidities like depression, anxiety, and migraines further increase vulnerability, making RLS more prevalent during menopause.
- OSA: During menopause, the risk of obstructive sleep apnea goes up, likely due to hormonal changes and potential weight gain. Sleep apnea causes breathing interruptions while you sleep, leading to poor-quality rest and leaving you feeling exhausted when you wake up. You may even feel more tired than when you went to bed!
- Mood disorders: Menopause often brings mood shifts, with many women experiencing increased anxiety or depression. These mood changes can make sleep even harder to achieve, creating a cycle where poor sleep worsens emotional well-being. Anxiety and depression can trigger insomnia, which then fuels more mood struggles, making restful sleep even more elusive.
How long do menopause-related sleep problems last?
If you’re dealing with menopause-related sleep disturbances, you’re likely wondering when you can finally enjoy a peaceful night’s rest again. While every woman’s experience is different, studies give us some insights into how long these challenges might persist.
Sleep difficulties often start during perimenopause and can last for years. Research, including the Study of Women’s Health Across the Nation (SWAN), shows that vasomotor symptoms (VMS), like hot flashes and night sweats, can last for an average of seven years. They might not go away right after menopause. In fact, the average length of frequent VMS after the final menstrual period (FMP) is 4.5 years.
Other factors can influence how long symptoms last:
- Earlier onset of VMS (during perimenopause or early perimenopause) is linked to longer durations, with some women experiencing symptoms for over 12 years.
- Women who were past menopause when hot flashes started experienced the shortest total duration of symptoms, about 3 years on average.
- African American women reported the longest average duration of symptoms (about 10 years) compared to other groups.
- Additional factors, such as higher stress levels, greater symptom sensitivity, anxiety, depression, and younger age at onset, are associated with longer-lasting symptoms.
While menopause-related sleep problems can last for several years, there are ways to improve your sleep quality during this time. From lifestyle adjustments to medical interventions, you have options.
Lifestyle changes that can improve sleep during menopause
Changes in your daily routine can make a difference in your sleep quality during menopause. Here are some lifestyle adjustments you might find helpful:
- Aim for a consistent sleep schedule: Try setting regular bed and wake-up times, even on weekends. This can help regulate your body’s internal clock and improve your overall sleep quality.
- Embrace regular movement: Add moderate exercise to your daily routine. Even a 30-minute walk can help improve your sleep and overall well-being. Remember, any movement is better than none!
- Create a sleep sanctuary: Keep your bedroom cool. Lightweight bedding and breathable fabrics could help you feel more comfortable throughout the night.
- Explore stress-management techniques: Try relaxation methods like gentle yoga or deep breathing before bed, which might help calm your mind. These practices can prepare your body for restful sleep.
- Be mindful of evening habits: Avoid heavy meals close to bedtime, and don’t drink too much liquid in the hours before you go to sleep.
Can hormone replacement therapy improve sleep quality during menopause?
Research shows that low-dose hormone replacement therapy (HRT) can significantly improve sleep quality. HRT replaces hormones that your body stops producing during menopause, helping to relieve symptoms like hot flashes, night sweats, and sleep disturbances. Note: HRT can also be referred to as MHT (menopause hormone therapy) and HT (hormone therapy).
A 2018 study in Menopause: The Journal of The North American Menopause Society found that women using low-dose HRT saw marked improvements in sleep quality over four years compared to those on a placebo.
There are two main types of HRT:
- Combined therapy, which includes both estrogen and progesterone
- Estrogen-only therapy, typically prescribed for women without a uterus
HRT is available in several forms, including:
- Oral tablets
- Skin patches
- Gels and creams
- Estradiol sprays
Which works best for sleep? A comprehensive study found that estrogen and combined therapy both improved sleep, with transdermal forms, like the patch, being particularly helpful.
Patches may provide a steadier hormone release, helping reduce sleep disruptions. HRT is also highly effective at reducing the frequency of hot flashes and night sweats, which in turn enhances overall sleep quality.
While HRT offers many benefits, it isn’t suitable for everyone. The Women’s Health Initiative (WHI) study raised concerns about HRT, linking it to increased risks of certain health conditions like heart disease and breast cancer. More research has clarified that these risks are largely dependent on factors like age, timing, and individual health conditions. As always, before starting HRT, be sure to share your personal health history with your doctor to determine if it’s suitable for you.
Are there any over-the-counter or herbal remedies for menopause-related sleep problems?
When menopause keeps you tossing and turning, it’s natural to eye over-the-counter (OTC) remedies, supplements, or herbal options. While some might offer a little relief, let’s talk about what really works and what doesn’t.
- Melatonin supplements: Melatonin is a hormone naturally produced by your brain. It acts as your body’s built-in “go-to-sleep” signal, helping regulate your sleep-wake cycle. Supplements can give it a boost, potentially helping you fall asleep faster and improve sleep quality. But let’s keep expectations in check—it’s not a magic fix. Research on its effects in menopausal women is mixed, and taking too much can leave you feeling groggy or with a headache. It’s best used sparingly, as a gentle nudge rather than a cure-all for sleep issues.
- Herbal teas: Sipping chamomile, valerian root, or passionflower tea before bed feels cozy and calming—and honestly, that bedtime ritual can be a win on its own. But when it comes to real science, evidence that these teas completely solve menopausal sleep problems is a little thin. They won’t hurt, though, and if they help you relax, that’s still a plus.
- Magnesium supplements: Magnesium, a mineral that supports muscle relaxation and nerve function, has been linked to improved sleep. Some research suggests it may help with sleep quality, especially in menopausal people. But magnesium alone won’t solve significant sleep problems. Consult a doctor before trying and stick to recommended amounts because high doses can upset your stomach.
- Black cohosh: Black cohosh gets a lot of hype for hot flashes and night sweats, and some women swear by it. But the science is iffy—some anecdotal reports show benefits, others don’t. Plus, it’s not FDA-regulated, so you’ll want to be cautious and talk to your doctor before giving it a try. It might help, but it’s far from a guaranteed fix.
OTC remedies and herbal options are helpers, not cures. They might ease symptoms, but they won’t address the root causes of menopause-related sleep issues. Everyone responds differently, so what works for your friend might not work for you—and that’s okay! Pairing these remedies with lifestyle changes, like a solid bedtime routine, stress management, and a sleep-friendly environment, can lead to better results.
Remember, you’re unique, and what works for one person might not work for another. At Noom, we’re here to help you find the right combination of lifestyle changes to improve your sleep during menopause. Together, we can develop a personalized plan that fits your needs and helps you feel your best.
Taking action: Improving sleep during menopause
Managing menopause-related sleep challenges can feel overwhelming, but small, consistent changes can make a big difference. Start by creating a regular sleep schedule, a calming bedroom environment, and relaxation techniques that work for you. Ask your doctor if HRT or other therapies might work for you. Remember, finding the right approach is personal and takes time.
At Noom, we’re here to guide you every step of the way. Our personalized tools and strategies help you build lasting habits for restful nights and energized days. Many women have improved their sleep and overall health with our comprehensive approach, which helps manage menopause symptoms like weight gain, stress, and sleep issues. Let Noom help you transform sleepless nights into restful ones and thrive during this stage and beyond.




 Melissa Kay
Melissa Kay
 Noom Team
Noom Team