Vitamin D is called the sunshine vitamin because as the skin absorbs the sun’s rays, a natural process produces it. It is also known as calciferol. Vitamin D is crucial for strong, healthy bones, proper functioning of muscles, heart, lungs, brain, and immune system. Besides vitamin D’s natural production, you can get the vitamin in supplement form and vitamin-enriched foods. Natural food sources of the vitamin are limited.
Recent research has uncovered that more people are deficient in vitamin D than once thought, so more and more enriched foods are hitting the market. How exactly does the body use vitamin D, and who benefits most from supplementation? Let’s take a look at this vitamin more closely.

Vitamin D and the Sun
The most natural way to get vitamin D is by exposing your bare, unprotected skin to the sun. It doesn’t take long to get what you need.
You only need to expose your skin for about 20-30 minutes at a time during the brightest part of the day. How much vitamin D you produce depends on the time of day, where you live, the current season, and your skin color. The more skin that you expose, the more of the vitamin that will be produced.
Direct sunlight is necessary for the body to produce vitamin D. You can’t sit next to a window in hopes of upping your body’s production. Unfortunately, the UV rays required to produce vitamin D can’t make it through the glass.
It is thought that the recent uptick in vitamin D insufficiency or deficiency is related to changes in activity levels. People spend more time indoors than ever before, and the best times of day to get outside, between 10 am and 3 pm, are when children are in school and adults are at work.
Even if the only function of vitamin D were to facilitate the absorption of calcium, that would be enough, but it does so much more.
What Does Vitamin D Do?
Before vitamin D can do anything in the body, it needs to go through two hydroxylations. The first hydroxylation changes the calciferol to calcidiol. This occurs in the liver. The calcidiol is then changed into calcitriol in the kidneys after the second hydroxylation. Once converted into the active form, vitamin D is utilized throughout the body to maintain homeostasis or balance. It’s this homeostasis that we often refer to as “good health.”
But, what exactly does this now active form of vitamin D do? First off, it “helps regulate the amount of calcium and phosphate in the body.” The connection between the vitamin and healthy bones was discovered when doctors recognized that sunlight helped prevent a bone condition known as rickets in children. They also realized that cod liver oil, which contains the vitamin, seemed to help. Low vitamin D affects adults, as well, but instead of rickets, a condition called osteomalacia may occur if levels fall too low.
“Vitamin D is important to the body in many other ways as well. Muscles need it to move, for example, nerves need it to carry messages between the brain and every body part. The immune system needs vitamin D to fight off invading bacteria and viruses. Together with calcium, vitamin D also helps protect older adults from osteoporosis.”
Real results with a personalized weight loss program
Take the quiz!

Vitamin D and:
Let’s take a closer look at the role vitamin D plays in the body and how it affects the disease process.
- Calcium Absorption
A significant role of vitamin D is in calcium absorption. “Vitamin D is the principal factor that maintains calcium homeostasis. Increasing evidence indicates that the reason for disturbed calcium balance with age is inadequate vitamin D levels in the elderly.” But, it’s not just the elderly. Insufficiency and deficiency of the vitamin are being noted across all age groups.
Calcium homeostasis is critical because it keeps “serum calcium levels within a narrow range.” “The intestine, kidney, bone, and parathyroid gland” play a part in serum calcium level regulation.

- Depression
According to the Journal of Affective Disorders, “there is adequate evidence for a positive association between vitamin D deficiency and depression.” Authors also state, “there is a need for further randomised controlled longitudinal studies.”
Researchers aren’t sure exactly how vitamin D alleviates depression. Elevated CA2+ levels may contribute to depression, so there’s some indication that vitamin D reduces these levels and thus treats depression. It appears the effect spans both unipolar and bipolar depression.
“… vitamin D deficiency may be associated with an increased risk or severity of depression. Supplementation of vitamin D may confer protection for depressed patients,” says research in Current Drug Targets.
Unfortunately, as it goes in clinical research, there’s also evidence that vitamin D has no impact on the course of the disease or remission rates. However, there may be a connection between the mortality rate in patients with depression and vitamin D status. Research shows increased mortality in people living with depression and low vitamin D levels.
- Cancer
Vitamin D “slows malignant cellular growth,” and research suggests that “ultraviolet-B exposure can help reduce cancer risk and prevalence, indicating a potential role for vitamin D as a feasible agent to prevent cancer incidence and recurrence.”
This slowing of malignant tumor growth has been shown in cases of colorectal cancer, breast cancer, and prostate cancer, with colorectal cancer research offering the most compelling results.
Just as was the case with vitamin D and depression, vitamin D’s effect on cancer is up for debate. According to the New England Journal of Medicine, a 2019 placebo-controlled trial showed, “supplementation with vitamin D did not result in a lower incidence of invasive cancer…”
- Diabetes
In a meta-analysis including more than 28,000 adults followed for more than seven years, there was a 31% increased risk of developing diabetes. Even when confounders that could skew risk were considered, there remained a 16% greater risk of diabetes in older adults who were vitamin D insufficient or deficient.
Supplementation would be the first defense line to counteract the insufficiency, so why not just take a vitamin D supplement as a prophylactic? “Among persons at high risk for type 2 diabetes” who did not have vitamin D insufficiency, “vitamin D3 supplementation at a dose of 4000 IU per day did not result in a significantly lower risk of diabetes than placebo.”
Looking at the potential use of vitamin D in diabetes from a different angle, researchers have shown that vitamin D may work to help regulate Ca2+ and reactive oxygen species levels (ROS). When pancreatic beta cells kick into overdrive to fight rising blood glucose levels, Ca2+ and ROS levels increase. This causes cellular death and, eventually, the onset of diabetes. “When vitamin D is deficient, many of these processes begin to decline, and this sets the stage for onset of diseases such as diabetes.”
It’s promising to find that some of the most recent research is in agreement as of 2020. Vitamin D plays a role in the prevention of type 2 diabetes. “Longitudinal observational studies report highly consistent associations between higher blood [vitamin D] levels and a lower risk of incident diabetes in diverse populations, including populations with prediabetes. Trials in persons with prediabetes show risk reduction in incident diabetes with vitamin D supplementation. In the 3 large trials that were specifically designed and conducted for the prevention of diabetes, vitamin D supplementation, when compared with placebo, reduced the risk of developing diabetes by 10% to 13% in persons with prediabetes not selected for vitamin D deficiency.”
Diabetes is one of the potential health concerns that come with obesity. If you want to lose weight and you’re tired of the same old song and dance, check out Noom – a unique psychological take on weight loss.
- Multiple Sclerosis
Multiple sclerosis (MS) is, in part, an inflammatory disease. Research has shown that vitamin D has an immunomodulatory effect in patients with MS who’re insufficient in the vitamin. While major clinical trials are still needed, researchers note, “robust statistical models used in five different association studies have already predicted a favorable vitamin D effect reducing relapses by 50–70%.”
Some research suggests a causal relationship between vitamin D insufficiency and deficiency and MS. Previously, much of the data surrounding the vitamin’s impact on the disease process was observational, but newer research uncovered a more clinically significant connection.
According to the American Academy of Neurology, there is “strong evidence that low serum [vitamin D] concentration is a cause of MS, independent of established risk factors.”
- Obesity
The relationship between vitamin D and obesity is just emerging. Vitamin D is a fat-soluble vitamin that’s stored in fat cells. Research has shown that obese individuals have significantly lower levels of serum vitamin D than do normal-weight counterparts. This effect is found across all ethnicities, ages, and geographical locations.
This is hugely important because “vitamin D plays a role in the adipogenesis process and inflammation status in adipocytes and adipose [fat] tissue.”
- Cardiovascular Disease
There’s a connection between low vitamin D levels, hypovitaminosis D, and increased cardiovascular disease risk. It appears that when vitamin D levels are low, calcification of blood vessel walls increases. These calcifications are common, but they do lead to an increased risk of blood clots and stroke.
Vitamin D levels may also play a role in hypertension, one of the most wide-spread cardiovascular conditions across the world. Multiple studies have shown that low levels of vitamin D are found in patients with high blood pressure. The risk of developing hypertension is also lower in individuals who are vitamin D-sufficient.

- Osteoporosis
According to the World Health Organization, osteoporosis is defined as a 50% reduction in bone mass and bony quality. We know vitamin D plays a crucial role in bone health, but what recent research has shown is that increasing vitamin D levels, in the case of osteoporosis, should be done nutritionally, not with supplements.
That’s not to say supplementing doesn’t work to fight osteoporosis, as well. In one study, after eight weeks of taking vitamin D supplements, participants who were vitamin D deficient at the start of the study significantly improved related bone density scores by the conclusion.
- Asthma
Vitamin D “deficiency has been associated with increased inflammation, exacerbations, and overall poor outcomes in patients with asthma. Given the increase in the prevalence of asthma over the past few decades, there has been enormous interest in the use of vitamin D supplementation as a potential therapeutic option.”
Unfortunately, the evidence surrounding vitamin D and asthma is mostly focused on children. Adult studies are lacking, and the ones that have been completed often report that further testing is needed to establish a relationship between low vitamin D and worse asthma control.
- Cognitive Function
In a study of more than 900 individuals aged 65 and over who were followed for 12 years, participants with low vitamin D levels were three times more likely to develop Alzheimer’s disease than their vitamin D-sufficient counterparts.
The inverse has also been shown in clinical research. A 2018 review of studies on dementia, Alzheimer’s, and vitamin D levels showed participants with higher serum vitamin D levels were less likely to develop either of the cognitive conditions.
- Fatigue
Studies into the effect of vitamin D levels and fatigue are on-going, with results falling on both sides of the debate. In some research, men and women who self-report fatigue and have low vitamin D levels, based on blood testing, report fatigue resolution using a vitamin D supplement. In one study, all it took was one high-dose of 100,000 IU of vitamin D to reduce overall fatigue test scores.
However, in 2019, another study reported that “vitamin D supplementation of the general population to raise [serum vitamin D] levels is not likely to be useful in preventing fatigue.”
- Immune Function
“The classical functions of vitamin D are to regulate calcium-phosphorus homeostasis and control bone metabolism. However, vitamin D deficiency has been reported in several chronic conditions associated with increased inflammation and deregulation of the immune system, such as diabetes, asthma, and rheumatoid arthritis. Together with experimental studies, these observations suggest a critical role for vitamin D in the modulation of immune function. This leads to the hypothesis of a disease-specific alteration of vitamin D metabolism and reinforces the role of vitamin D in maintaining a healthy immune system.”
- Rickets
“The epidemic scourge of rickets in the 19th century was caused by vitamin D deficiency due to inadequate sun exposure and resulted in growth retardation, muscle weakness, skeletal deformities, hypocalcemia, tetany, and seizures.”
Rickets can be prevented with proper nutrition. “Prevention of nutritional rickets can be achieved by ensuring that pregnant women and infants receive regular supplements of vitamin D. Vitamin D supplementation of infants should be regarded as having a similar level of importance as immunisation.”
Treatment for rickets includes calcium and vitamin D supplementation. “Daily calcium intakes of 1000 mg or 2000 mg produced more rapid radiographic healing of rickets than 500 mg, but 2000 mg did not have greater benefit than 1000 mg.” It can take months for rickets to resolve with “Some children requir[ing] longer than 24 weeks for complete healing of nutritional rickets.”
While nutritional rickets is the most common variety, there is a genetic condition called hypophosphatemia “characterized by low circulating concentrations of phosphorus that impair skeletal mineralisation.” This “results in rickets in growing children and osteomalacia in adults.”
- Osteomalacia
“Osteomalacia results from nutritional deficiencies, abnormal collagen matrix, abnormal alkaline phosphatase activity, or inhibitors of mineralization. The incidence of osteomalacia is increasing despite public health measures in the mid-twentieth century that markedly decreased its prevalence.”
Medications and genetic factors, and nutritional vitamin D deficiency, can cause the softening of bones, so clinical examination, blood tests, imaging, and bone biopsy may be necessary to rule out nutritional deficiency.
Nutritional osteomalacia typically affects the aging population for various reasons, including poor diet and lack of sun exposure. Treatment includes calcium and vitamin D supplementation for at least one year. In some cases, it will take longer than one year to heal completely.

- Athletics
In the past three years alone, there has been an influx of research into vitamin D status and athletes. Because vitamin D plays a crucial role in skeletal muscle function, it’s understandable how a connection between performance and vitamin D deficiency or insufficiency could be made.
First and foremost, research shows that more than 50% of athletes have inadequate levels of vitamin D in the blood. Numbers tend to increase in winter months when UV rays are at their weakest.
And this study may have under-reported the issue. Another bit of research studying vitamin D levels in athletes showed that 70% of the 128 trained athletes recruited presented with low blood concentrations of vitamin D.
According to the journal Hormones, vitamin D supplementation in deficient and insufficient athletes promotes the growth and development of type IIA muscle fibers. These fast-twitch fibers cause “an increase in muscular high power output.”
There’s also evidence that taking vitamin D supplements may improve “lower limb muscle strength in athletes.” Though, the same effect was not seen on upper limb muscle strength in the same study.
- Covid-19
Doctors worldwide are searching for every bit of information they can find on how Covid-19 works in the body and why some people are more strongly affected by the virus than others. Research has shown that Covid-19 patients with a lower serum vitamin D level often face a poorer prognosis than patients with sufficient vitamin D.
Some research also indicates that vitamin D may help reduce infection risk of Covid-19 and/or influenza. “To reduce the risk of infection, it is recommended that people at risk of influenza and/or COVID-19 consider taking 10,000 IU/d of vitamin D3 for a few weeks to rapidly raise 25(OH)D concentrations, followed by 5000 IU/d.”
Authors of one study in the Journal of Infection and Public Health agree. “… people who are at higher risk of vitamin D deficiency during this global pandemic should consider taking vitamin D supplements to maintain the circulating 25(OH)D in the optimal levels (75–125 nmol/L).”
Vitamin D Insufficiency and Deficiency
Vitamin D insufficiency and deficiency are serious health problems. Severe lack of the vitamin may cause a condition called rickets in children. It also can cause osteomalacia in adults. Both of these conditions cause soft, thin, and brittle bones.
Vitamin D deficiency is associated with cancer, asthma, diabetes, heart disease, hypertension, depression, Alzheimer’s, multiple sclerosis, and Crohn’s disease.
In most cases, adults have no idea they are insufficient or deficient in the vitamin. Common symptoms include mood changes, bone loss, muscle cramps, muscle weakness, bone and joint pain, and fatigue.
Young people and those with lighter skin can produce vitamin D from sunlight far better than people who have darker skin or are over 50 years of age. Because sunlight is the number one source of vitamin D in humans, planned time in the sunlight, without sunscreen, is one way of assuring you’re getting enough vitamin D. However, due to the increased potential for premature skin aging and skin cancer associated with direct sunlight exposure, more and more people are avoiding direct sunlight, which could be a partial cause of growing insufficiency.
What causes vitamin D deficiency?
It is thought that changes in how we live in modern times is one contributing factor to widespread vitamin deficiency or insufficiency. This is because fewer people spend time outdoors. Up “to 90% of vitamin D is absorbed through the skin via sunlight while the rest comes from the diet.” It is estimated that “twenty minutes of sunshine daily with over 40% of skin exposed is required to prevent vitamin D deficiency.”
Based on various studies, the best times to get sun exposure is between 10 am and 3 pm daily. Of course, seasonal changes cause reduced UV during fall and winter months, which means spending more than the recommended 20 minutes in sunlight during these times of the year.
Another cause of vitamin D insufficiency and deficiency relates to diet. As we age, vitamin D absorption may be limited, and older people may not be as apt to consume vitamin D-rich foods or enriched food products.
Who is at risk for vitamin D deficiency?
According to MedlinePlus.gov, people who’re at increased risk of vitamin D deficiency include:
- Infants who are breastfed
- Older adults
- People with more skin melanin or darker skin
- People with disorders that affect how the body processes fats (vitamin D is a fat-soluble vitamin)
- Obese men and women
- People post gastric bypass
- People with liver disease, kidney disease, or osteoporosis
- People with granulomatous diseases
- People taking medications that inhibit the metabolism of vitamin D

What is rickets?
Rickets is a childhood disorder caused by insufficient vitamin D. Vitamin D regulates calcium and phosphorus levels in developing bone. Without enough vitamin D, bone cannot take up the calcium it needs to form healthy, hard bone. The most common cause of rickets is a diet that lacks vitamin D, so it’s often called nutritional rickets.
The primary symptom of rickets is bowing or bending of the legs. This is caused by the pressure placed on soft bones when walking. In infants who’re crawling, a widening of the arm just above the wrist often develops.
Children at the highest risk of developing nutritional rickets are breastfed infants. Human milk lacks vitamin D, which is why infant vitamins typically supply 400 IUs of vitamin D to ensure proper bone growth. Breastfeeding moms may also need to supplement with vitamin D. Some sources suggest taking between 600 and 2000 IUs daily.
What is osteomalacia?
Osteomalacia is a bone disorder caused by vitamin D deficiency. In children, the condition is called rickets. While children present with a bowing of weight-bearing bones, like the legs, adults tend to present with fractures.
Typically, several factors come into play in developing osteomalacia in adults, including poor diet and lack of exposure to the sun or UV rays. However, there are health conditions that can affect how the body absorbs and uses vitamin D. Celiac disease, for instance, may cause damage to the intestinal lining, which impacts the absorption of vitamin D. Because the kidney and liver are required to convert vitamin D to its usable form, any conditions affecting the liver and kidney can also affect vitamin D levels.
The symptoms of osteomalacia include an aching pain that starts around the hips and spreads to the lower back, pelvis, and legs. In extreme cases, when calcium levels are at critically low levels, numbness and spasms in limbs and irregular heartbeat may occur.
The aging population and people who don’t have access to sunlight regularly are at the highest risk of osteomalacia.
Noom uses a unique green, yellow, red system to help you choose the most nutritious meals. This means getting all the vitamins you need from natural food sources.
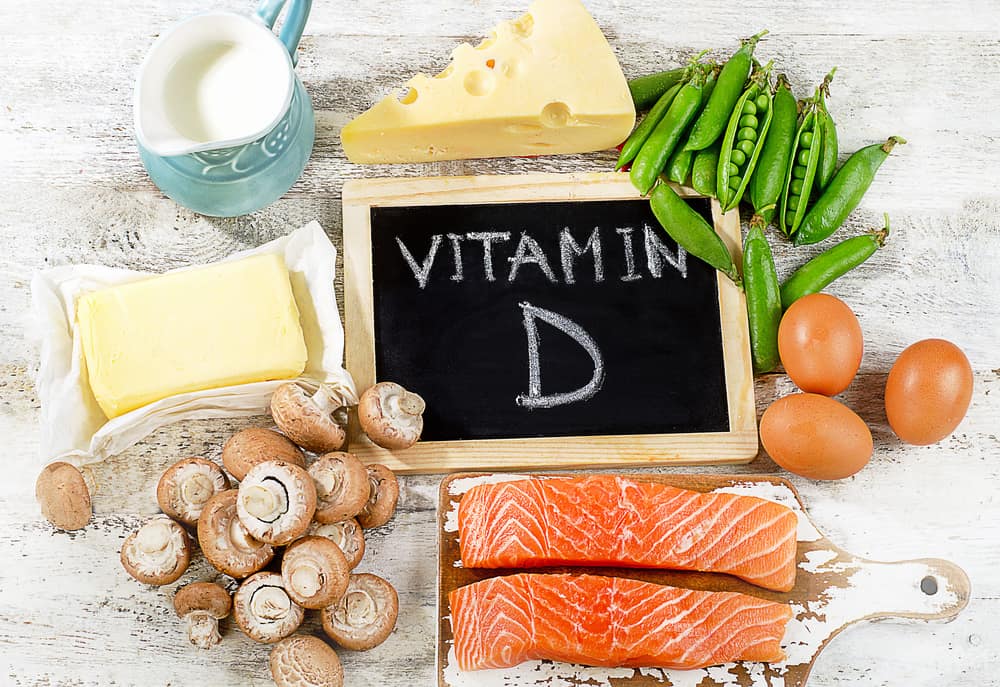
Vitamin D Food Sources
There are only a few foods high in vitamin D. Foods that contain vitamin D are mainly animal-based products, though mushrooms exposed to sunlight or UV rays are also excellent sources.
Food with the highest concentration of vitamin D include:
Salmon: A 6-ounce portion of cooked sockeye salmon supplies 142% of daily value (DV). If you’re eating farmed Atlantic salmon, that same 6-ounce portion provides 111% of DV. You can even use canned salmon, which supplies up to 90% of DV per three-ounce serving.
Mushrooms: One cup of raw cremini mushrooms packs 139% of DV, while a cup of diced portobellos comes in a close second with 122% of DV. Next are maitake and white button mushrooms, supplying 98% and 92% of DV per cup, respectively.
Other Fish: Atlantic mackerel supplies 90% of DV per fillet. Cooked swordfish offer significantly less vitamin D supplying only 71% of DV per three-ounce serving. Rainbow trout comes in at about 65% of DV per fillet, but it’s cod liver oil that takes the prize. It takes just one teaspoon of cod liver oil to supply more than 50% of DV of vitamin D. You can even try canned tuna, which delivers 34% of DV in one 3.5-ounce serving.
Milk: Whether you’re drinking whole, reduced-fat, or skim cow’s milk, you will gain between 29% and 32% of DV per 16-ounce serving. Soy milk falls in line with a supply of 29% of DV per 16-ounce serving.

Vitamin D Dosage
Vitamin D levels above 20 or 30ng/ml are considered healthy. However, it is estimated that more than 40% of people are deficient in the vitamin. “Vitamin D deficiency and insufficiency is a global health issue that afflicts more than one billion children and adults worldwide.” Deficiency has been associated with acute and chronic illnesses like autoimmune disorders, cardiovascular disease, infectious diseases, cancers, type 2 diabetes, and more.
The risk of vitamin D deficiency increases for:
- Children
- Pregnant and nursing women
- Obese people
- Darker-skinned people
- People with certain health conditions
It’s important to note that for most people, the term deficiency doesn’t apply. Vitamin D deficiency assumes health problems have occurred related directly to low vitamin D levels. Insufficiency is a better term, as people aren’t getting enough of the vitamin, but health problems aren’t prevalent in all cases.
Recommended Doses of Vitamin D
The recommended dose of vitamin D varies by age and other factors, but generally speaking:
- Age 0 to 1 year: 10mcg or 400 IU daily
- Age 1 to 70 years: 15mcg or 600 IU
- Age 71 and older: 20mcg or 800 IU
- Pregnant or nursing women: 15mcg or 600 IU
Because fat stores the vitamin, obese people may need to double or triple the usual dose to reach adequate blood serum levels.
Did you know Noom works to ensure you’re getting the best quality nutrition by educating you on choosing the healthiest foods?
Vitamin D Side Effects and Toxicity
Even though so many people are considered insufficient in vitamin D, you can get too much. This most often occurs in people using vitamin D supplements as the human body can turn off vitamin D production in sunlight to protect against getting too much.
Vitamin D side effects may include:
- Elevated blood calcium levels
- Nausea
- Poor appetite
- Stomach pain
- Constipation
- Diarrhea
In extreme cases, vitamin D toxicity may occur. This is a rare but severe condition when you have too much of the vitamin in your body. It is usually a result of excessive long-term intake of the vitamin. There’s no evidence that taking one large dose will cause toxicity, and some clinical trials have used single doses of 100,000 IUs or more, which supports this claim.
Blood serum levels of around 30ng/ml are considered sufficient, but in cases of toxicity, concentrations have been reported “ranging between 150 and 1220 ng/ml.”
Because of the increased awareness surrounding vitamin D insufficiency, more vitamin D blood tests are being ordered, leading to healthcare providers suggesting vitamin D supplementation. Overcorrection due to consistent overdosing is thought to be one of the primary causes of vitamin D toxicity.
Researchers estimate that around 75% of all reports of vitamin D toxicity have been made since 2010, with most cases being “a consequence of inappropriate prescribing, and the use of high-dose over-the-counter preparations or unlicensed preparations.”
According to Frontiers in Endocrinology, “Increased public awareness of vitamin D–related health benefits might increase the risk of VDT due to self-administration of vitamin D in doses higher than recommended for age and body weight or even higher than the established upper limit intake values. Consequently, the incidence of hypercalcemia due to hypervitaminosis D might increase.”
Bottom Line on Vitamin D
Vitamin D is a critical vitamin to overall health and well-being. This vitamin is about way more than bone health. With the rising number of people living with lower than ideal vitamin D levels, a stronger focus on nutrition and lifestyle changes to increase vitamin D exposure is necessary. While you can add some vitamin D-rich foods to your diet, the best way to get more is by simply going outside each day and soaking up the sun’s rays.
At Noom, we encourage daily exercise to get your body moving because moving more burns more calories, and, with Noom, the more you move, the more calories you can eat each day. Check out the program today!
Questions and Answers on Vitamin D
What foods are high in vitamin D?
Few foods are high in vitamin D. Fish contains the highest concentration of the fat-soluble vitamin, but mushrooms exposed to sunlight or UV come in a close second.
What does vitamin D do?
Vitamin D plays a critical role in phosphate and calcium levels in the body. Having enough of the vitamin is necessary for bone, muscle, and teeth health. There’s also evidence vitamin D affects cognitive and cardiovascular health, among others.
How can I increase my vitamin D level?
The most effective way to increase vitamin D levels is with direct sunlight. While you can take too much vitamin as a supplement, the body stops vitamin D production when levels are optimal to prevent toxicity. If you spend between 20 and 30 minutes in direct sunlight with at least 40% of your skin uncovered and unprotected by sunscreen, that should be enough to meet daily vitamin D requirements.
What happens when your vitamin D is low?
When your vitamin D is low, you may experience fatigue, bone pain, muscle weakness, and mood changes. These symptoms are common among many medical conditions, so vitamin D insufficiency is not often the first thought.
Are vitamin D and D3 the same thing?
Vitamin D3 is a form of vitamin D sourced from animals. Vitamin D2 is sourced from plants.
Are vitamin D supplements safe?
Vitamin D supplements are generally considered safe. Side effects and toxicity are associated with excessive intake of supplemental vitamin D over time.
Are there any vitamin D side effects?
Some of the side effects of too much vitamin D include elevated blood calcium levels, nausea, poor appetite, stomach pain, constipation, and diarrhea.
Can vitamin D cause constipation?
In some cases, high doses of vitamin D may cause constipation.
Do I have to take calcium with vitamin D?
Real results with a personalized weight loss program
Take the quiz!

No, you do not have to take calcium with vitamin D. Your body needs vitamin D to absorb calcium, but it does not need calcium to absorb vitamin D.
Will vitamin D help you lose weight?
Some research suggests a link between increasing vitamin D intake and weight loss. In one study, after one year of following the same diet and exercise program, participants who took a vitamin D supplement lost seven pounds more, on average, than participants who didn’t take the vitamin.